The most significant hazard associated with splinting is a critical concern in medical treatment, posing potential risks to patient safety. This comprehensive guide delves into the nature of this hazard, exploring its causes, risk factors, and evidence-based strategies for prevention and mitigation.
Splinting plays a vital role in immobilizing injured or unstable body parts, promoting healing and recovery. However, improper use or prolonged application can lead to a range of complications, including pressure sores, nerve damage, and impaired circulation.
Introduction
Splinting is a medical procedure that involves immobilizing a body part or joint to promote healing, prevent further injury, or correct deformities. While splinting is generally safe and effective, there is one significant hazard associated with its use.
The most significant hazard associated with splinting is skin breakdown, which can occur due to prolonged pressure, friction, or moisture buildup under the splint. Skin breakdown can range from minor skin irritation to serious pressure ulcers, which can lead to infection and other complications.
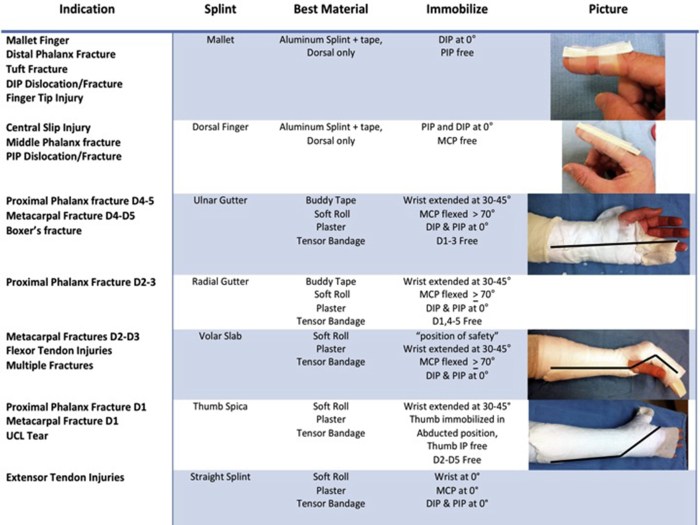
Types of Splints
There are various types of splints used in medical settings, each designed for specific purposes and body parts. The type of splint can impact the potential hazards associated with its use.
- Rigid splints: Made of hard materials like plaster or fiberglass, rigid splints provide maximum immobilization but can be bulky and uncomfortable.
- Semi-rigid splints: Made of materials like thermoplastic or aluminum, semi-rigid splints offer a balance between immobilization and flexibility.
- Soft splints: Made of soft materials like foam or fabric, soft splints provide minimal immobilization but are comfortable and allow for some movement.
The choice of splint type depends on the specific condition being treated, the level of immobilization required, and the patient’s comfort level.
Causes of Skin Breakdown
Skin breakdown associated with splinting can be caused by several factors:
- Prolonged pressure: When a splint is applied too tightly or for an extended period, it can exert excessive pressure on the skin, leading to tissue damage and skin breakdown.
- Friction: Movement of the skin against the splint’s surface can create friction, causing irritation and skin damage.
- Moisture buildup: Splints can trap moisture under them, creating a moist environment that promotes bacterial growth and skin breakdown.
These factors can interact and exacerbate the risk of skin breakdown, especially in patients with sensitive skin or underlying medical conditions that affect skin integrity.
Risk Factors
Certain factors can increase the risk of experiencing skin breakdown associated with splinting:
- Age: Elderly patients have thinner skin and reduced circulation, making them more susceptible to skin breakdown.
- Medical conditions: Patients with diabetes, peripheral vascular disease, or other conditions that affect skin health are at higher risk.
- Skin sensitivity: Individuals with sensitive skin or allergies are more prone to skin irritation and breakdown.
- Nutritional status: Malnutrition can impair skin integrity and increase the risk of skin breakdown.
Healthcare professionals should consider these risk factors when assessing patients for splinting and implementing preventive measures.
Prevention and Mitigation Strategies
There are several evidence-based strategies to prevent and mitigate the risk of skin breakdown associated with splinting:
- Proper fit and padding: Splints should be fitted correctly to avoid excessive pressure and friction. Padding can be used to protect bony prominences and areas prone to skin breakdown.
- Skin assessment: Regular skin assessments are crucial to identify any early signs of skin irritation or breakdown. Prompt intervention can prevent further damage.
- Moisture management: Keeping the skin under the splint dry is essential. Moisture-wicking materials and frequent dressing changes can help reduce moisture buildup.
- Pressure relief: Regularly removing the splint and elevating the affected limb can help relieve pressure and promote circulation.
These strategies have been shown to effectively reduce the risk of skin breakdown and improve patient outcomes.
Monitoring and Evaluation
Patients using splints should be closely monitored to identify and address any potential hazards:
- Regular skin assessments: Healthcare professionals should perform regular skin assessments to detect any signs of skin irritation or breakdown.
- Patient education: Patients should be educated on the signs and symptoms of skin breakdown and instructed to report any concerns promptly.
- Evaluation of prevention and mitigation strategies: The effectiveness of prevention and mitigation strategies should be evaluated regularly to ensure they are working effectively.
By implementing these monitoring and evaluation measures, healthcare professionals can ensure the safe and effective use of splints.
FAQ Insights: The Most Significant Hazard Associated With Splinting Is
What is the most common type of splinting hazard?
Pressure sores are the most common type of splinting hazard, occurring when excessive pressure is applied to a localized area of skin.
What are the risk factors for splinting hazards?
Risk factors include prolonged splinting, poor skin condition, malnutrition, and impaired circulation.
How can splinting hazards be prevented?
Prevention strategies include using the appropriate type of splint, applying it correctly, monitoring patients closely, and educating them on proper care.